A Holistic Approach to Personal Well-Being at F7 Wellness
F7 Wellness aims to redefine the concept of personal well-being and offer a truly holistic approach to wellness. Their commitment to redefining wellness is made possible through the application of InBody, to provide clients with comprehensive insights into their body composition and overall health. Unlike traditional methods that rely solely on weight and BMI, InBody utilizes Bioelectrical Impedance Analysis (BIA) technology to provide a detailed analysis of muscle, fat, and water distribution throughout the body. These body composition data empower individuals to make informed decisions about their health, enabling them to set realistic goals, track progress accurately, and make targeted adjustments to their wellness routines.
In this blog post, we will delve into the comprehensive use of InBody technology at F7 Wellness and how InBody transforms the wellness journey for their clients.

Advanced Technology for Comprehensive Analysis with the InBody970
Before each consultation session at F7 Wellness, clients will receive an InBody970 full-body composition analysis, a new state-of-the-art body composition technology from InBody. The printed InBody Body Composition Result Sheet will serve as a comprehensive guide, offering informative details about muscle and fat distribution, water balance both inside and outside cells as well as the overall health of body cells.
According to Dr Jassica, the F7 Wellness Doctor, this quick, convenient, and non-invasive analysis provides valuable insights into body composition and overall health, paving the way for a truly personalized wellness journey.
Alongside the body composition analysis, she reveals that the center also utilizes a fully automated blood pressure monitor, BPBIO750 for precise blood pressure measurements. This additional layer of screening enables the identification of potential risks associated with high blood pressure, ensuring a thorough understanding of each individual’s health condition.

 Application of InBody Parameters in Providing Personalized Nutrition Consultations
Application of InBody Parameters in Providing Personalized Nutrition Consultations
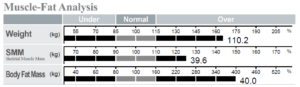
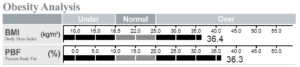
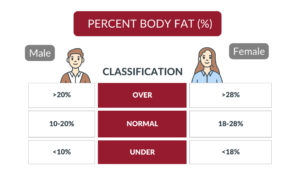
Following the body composition analysis, Dr Jassica will conduct a thorough review of the body composition data and also a comprehensive nutritional consultation. During nutritional consultations, she utilizes InBody parameters such as Body Fat Mass, Percent Body Fat, and Visceral Fat Area to screen for potential health risks that are associated with obesity and high visceral fat. For example, hypertension, diabetes, dyslipidemia, and fatty liver.

Going beyond the traditional focus on body fat, Dr. Jassica highlights InBody technology for its unique ability to provide clients with a deeper understanding of cellular health and nutritional status by looking at Phase Angle. Phase Angle measures the angle of resistance on cellular membrane, and it is often used as an indicator of cellular health and nutritional status. A higher Phase Angle is generally associated with better cellular health and nutritional status; meanwhile, a lower Phase Angle may indicate malnutrition or other health problems.
Moreover, with the InBody Evaluation Result Sheet, Dr Jassica now takes it a step further by educating clients on how their Phase Angle compares to populations of the same age and even those younger. This comparative analysis serves as a powerful motivational tool, igniting a sense of determination within clients to prioritize their well-being. By understanding where they stand in the spectrum of cellular health, clients are inspired to adopt behaviors and habits that support and enhance their cellular vitality, thus embarking on a journey towards improved overall wellness.
Following a thorough understanding of clients’ body composition and health conditions, the next step is to provide personalized nutritional advice and education on practicing a balanced diet.
Application of InBody Parameters in Tailoring Training Regimes
According to Lewis, the F7 Wellness Personal Trainer, he delves into InBody parameters like Percent Body Fat, Skeletal Muscle Mass, and Visceral Fat Area, to accurately assess clients’ fitness level and physical condition.
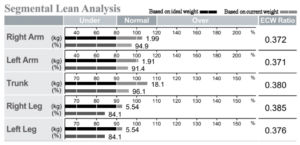
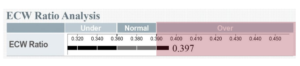
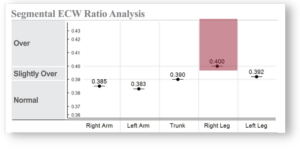
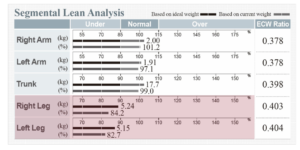
Alongside analyzing key metrics related to body fat, he fine-tunes the training regimen by assessing muscle balance through Segmental Lean Analysis (SLA) and muscle quality through ECW Ratio. ECW Ratio is an important indicator of body water balance, which measures the proportion of extracellular water (the fluid outside cells) to total body water (the combined amount of water inside and outside cells). An increase in ECW can sometimes indicate underlying issues or unusual conditions such as water retention, injury, or inflammation, which indirectly affect muscle quality.
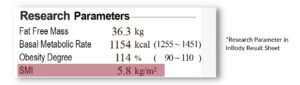
Furthermore, in the ongoing battle to prevent and manage sarcopenia, he also prioritizes monitoring Skeletal Muscle Index (SMI) for preserving muscle strength and enhancing clients’ quality of life as they age.

Wellness Redefined: Benefits of Integrating InBody in your Wellness Center
- Objective Tracking of Progress: InBody analysis provides objective metrics for tracking progress over time. Clients can see changes in their body composition, muscle mass, and fat levels, which can serve as motivation to adhere to their wellness plans.
- Enhanced Client Engagement: Incorporating InBody analysis into wellness programs can enhance client engagement by providing tangible data and visual representations of progress. Clients are more likely to stay committed to their wellness journey when they can see measurable results.
- Educational Opportunities: InBody can be used as an educational tool to help clients understand the importance of maintaining a healthy body composition and the impact it has on overall health and well-being. Wellness centers can use InBody results to educate clients about nutrition, exercise, and lifestyle choices.

Conclusion
The integration of InBody technology in wellness centers marks a pivotal advancement in the realm of health and fitness. By providing detailed and accurate body composition analysis, it not only enables the early identification of potential health risks but also facilitates the development of targeted interventions such as personalized nutritional advice and tailored training regimes. This holistic approach not only addresses immediate concerns but also fosters long-term health improvements, empowering clients to make informed decisions and achieve their wellness goals.
Watch our video below to discover how our InBody technology can elevate your clients’ wellness experiences at your wellness center. Together, we can empower your clients to take control of their health and achieve their wellness goals like never before!





 Meanwhile,
Meanwhile, 
 healthy growth and development!
healthy growth and development!















 2. Setting Data-Driven Goals: InBody analyzers are not just diagnostic tools; they are integral to rehabilitation and recovery programs. Healthcare providers can use InBody data to set measurable goals for muscle mass improvement and to tailor interventions like nutritional plans and physical therapy regimes.
2. Setting Data-Driven Goals: InBody analyzers are not just diagnostic tools; they are integral to rehabilitation and recovery programs. Healthcare providers can use InBody data to set measurable goals for muscle mass improvement and to tailor interventions like nutritional plans and physical therapy regimes.