*This webpage content is intended for Healthcare Professionals only, not for general public.
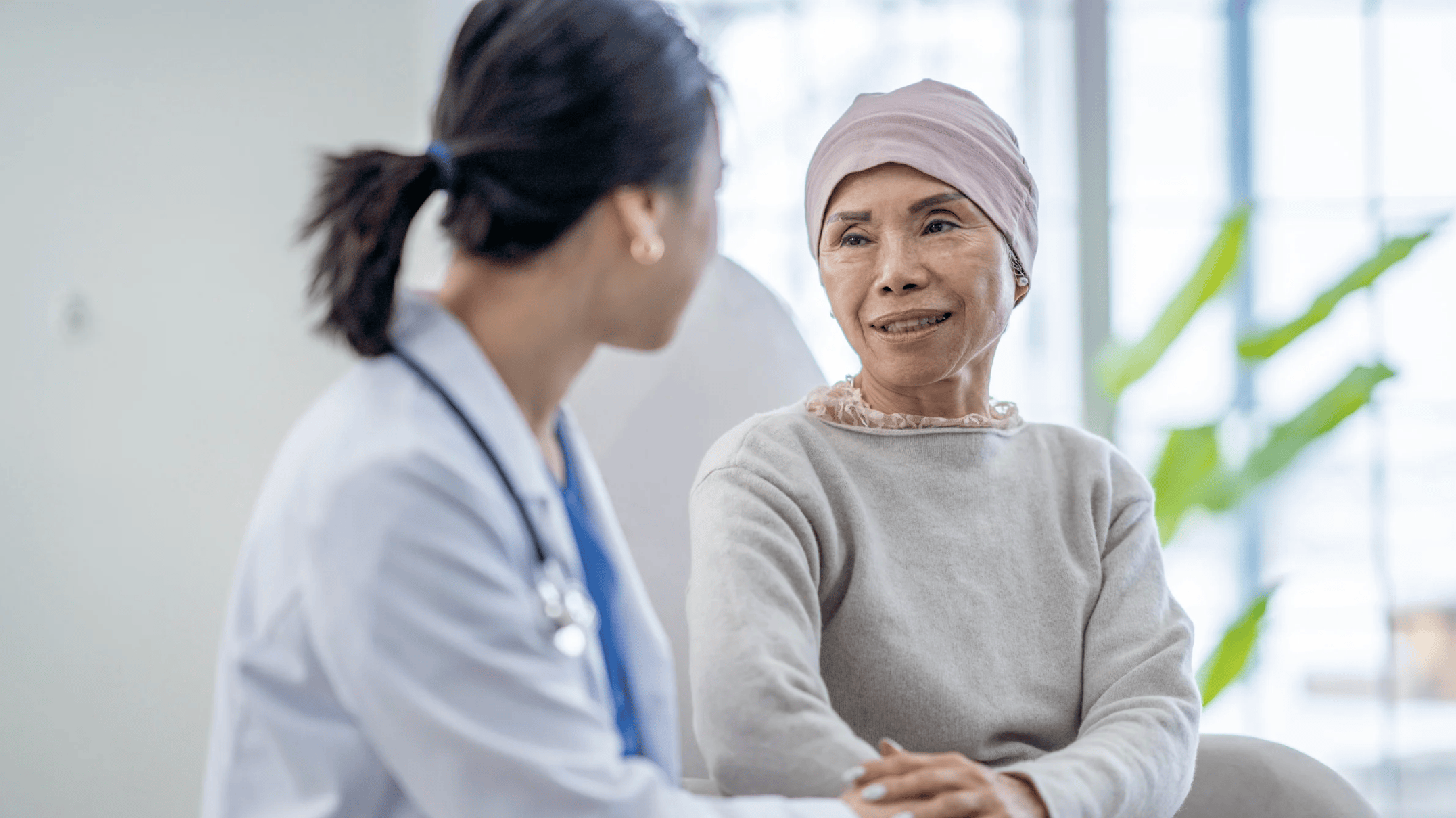
Every year on World Cancer Day (4 February), we are reminded that cancer care goes far beyond diagnosis and treatment alone. Nutrition, physical function, and overall body health play a crucial role throughout the cancer journey — from diagnosis to treatment, recovery, and continuum of care.
One key area that is often overlooked is body composition. While body weight is commonly monitored, it does not tell the full story of what is happening inside the body. This is where body composition analysis becomes a valuable tool in cancer care.
Why Weight Alone Is Not Enough in Cancer Management
In clinical practice, body weight is often one of the first parameters measured. However, in cancer care, weight alone can be misleading. Patients may maintain a stable body weight while experiencing profound internal changes that directly affect treatment outcomes and quality of life.
For example, loss of skeletal muscle mass may be masked by preserved or increased fat mass, or by fluid retention. Conversely, rapid weight loss may reflect not only fat loss but also critical muscle wasting.
Clinical research has shown that cancer patients may experience:
- Loss of skeletal muscle mass due to systemic inflammation, reduced physical activity, and treatment-related side effects
- Lower phase angle, reflecting impaired cell membrane integrity and reduced cellular function
- Disrupted body water balance caused by inflammation, malnutrition, or treatment-related edema
These changes are often invisible on the scale, reinforcing the need for more comprehensive body composition assessment in cancer care.
The Role of InBody in Cancer Management
InBody Body Composition Analysers provide a comprehensive assessment of body composition using Direct Segmental Multi-Frequency Bioelectrical Impedance Analysis (DSM-MFBIA). This approach enables the reporting of multiple clinically meaningful parameters that supports oncology care across treatment, recovery, and rehabilitation.
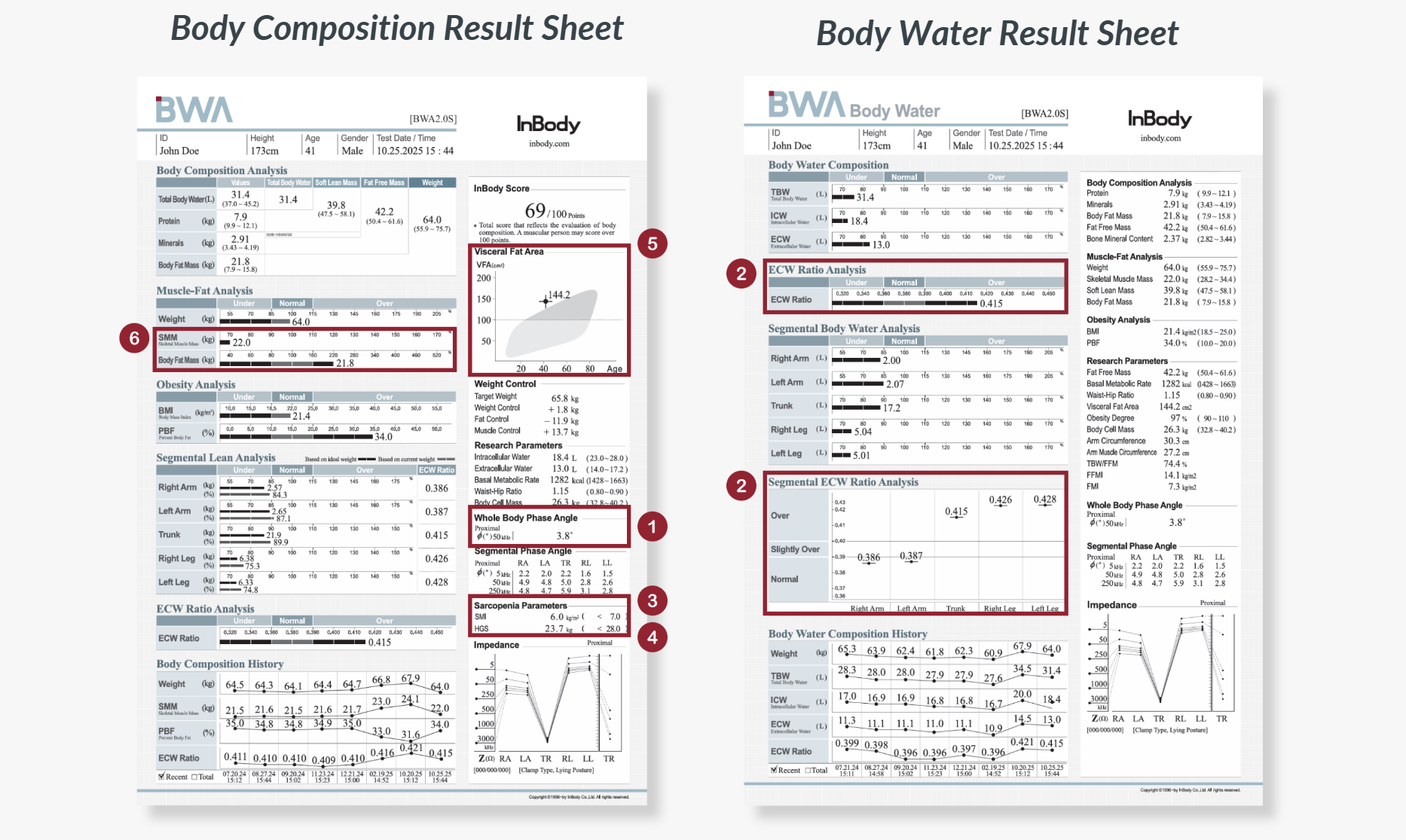
1. Phase Angle
Phase Angle serves as an indicator of cellular health and nutritional status. By assessing Phase Angle, clinicians and dietitians can identify malnutrition risks in cancer patients, tailor interventions, and monitor the effectiveness of immunotherapies.
2. Extracellular Water (ECW) Ratio
Cancer can cause muscle loss and compromise organ and cellular functions, resulting in systemic inflammation or edema. Monitoring the ECW Ratio allows oncologists to track fluid changes throughout the body and better understand the causes of imbalanced fluid levels. Segmental ECW Ratio analysis can detect specific areas of fluid retention that may go unnoticed with general assessments.
3. Skeletal Muscle Mass Index (SMI)
Cancer and its treatments contribute to muscle loss, making it crucial to screen for sarcopenia. SMI identifies patients at risk, allowing interventions to preserve muscle health and support physical function.
4. Handgrip Strength (HGS)
HGS is a simple yet effective measure of muscle function and strength. In oncology patients, it complements SMI by assessing functional muscle performance, helping clinicians evaluate sarcopenia risk.
5. Visceral Fat Area
Visceral fat reflects the hidden fat stored around internal organs. Excess visceral fat is associated with chronic inflammation and metabolic complications, which may negatively influence cancer outcomes, treatment response, and recovery. Assessing visceral fat area provides additional insight beyond body weight or BMI, supporting more targeted risk assessment and management.
6. Muscle-Fat Analysis
Disease onset, progression, and treatment can shift body composition, especially leading to muscle loss. Assessing muscle-fat balance is essential, as low muscle mass is linked to poorer survival rates and reduced treatment tolerance.
Conclusion
Body composition analysis reveals the full picture of a patient’s health, going far beyond what weight alone can show. By performing InBody Body Composition Analysis, clinicians can make informed decisions, personalize care, and track progress throughout the cancer journey.
With these insights, patients and healthcare teams alike can take meaningful steps toward stronger, healthier outcomes — because understanding your body is the first step to taking control of your recovery.