*This webpage content is intended for Healthcare Professionals only, not for general public.
Setting a Global Standard for Malnutrition Diagnosis
Malnutrition remains a serious but often underdiagnosed condition that affects patients across all healthcare settings — from hospitals to long-term care facilities. Recognizing the need for a universal diagnostic framework, the Global Leadership Initiative on Malnutrition (GLIM) was established in 2016 by representatives from four major global clinical nutrition societies:
- ESPEN (Europe)
- ASPEN (United States)
- FELANPE (Latin America)
- PENSA (Asia)
Together, they set out to build a global consensus for diagnosing malnutrition in adults in clinical settings. This initiative aims to provide clinicians worldwide with a standardized, evidence-based framework to improve nutrition care.
The GLIM Diagnostic Criteria
GLIM recommends that malnutrition diagnosis begins by confirming at least one phenotypic and one etiologic criterion.
Etiologic Criteria
These highlight the underlying causes of malnutrition:
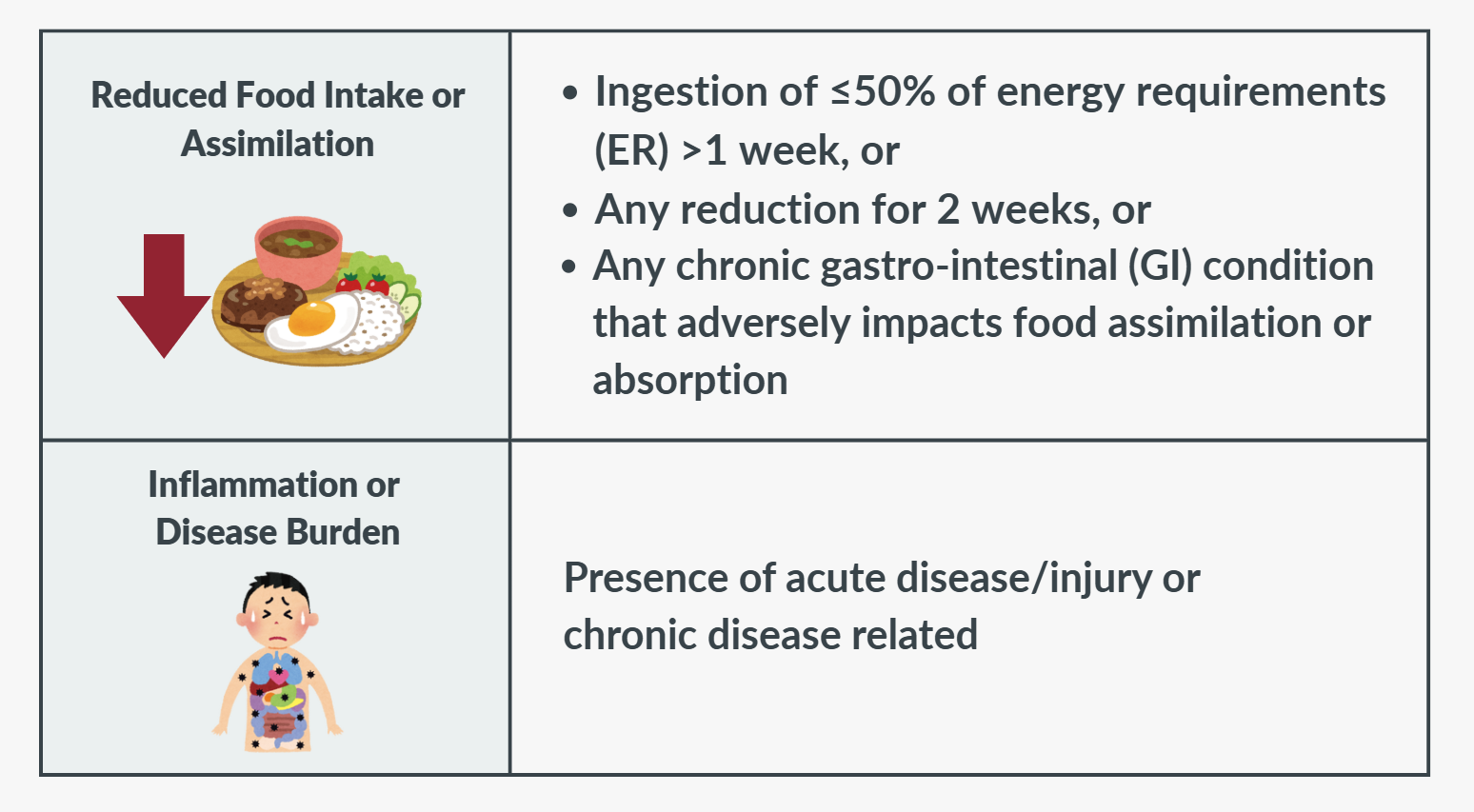 1. Reduced Food Intake or Assimilation
1. Reduced Food Intake or Assimilation
Malnutrition may result from poor appetite, illness, medication use, psychological conditions, or difficulties in chewing, swallowing, or nutrient absorption. GLIM defines this criterion as intake 50% and below of energy needs for more than one week, any intake reduction lasting over two weeks, or chronic gastrointestinal disorders affecting absorption.
2. Inflammation or Disease Burden
Many diseases trigger inflammatory responses that accelerate muscle breakdown, suppress appetite, and alter metabolism, all of which contribute to malnutrition. GLIM recognizes both acute (e.g., infection, injury) and chronic (e.g., cancer, organ failure) inflammatory conditions as valid causes.
While laboratory tests like C-reactive protein (CRP) can confirm inflammation, GLIM emphasizes that clinical judgment often suffices when inflammation is evident from the patient’s condition. Repeated CRP measurements above the normal threshold can further support the diagnosis of chronic inflammation.
Phenotypic Criteria
These describe the physical signs and measurable changes associated with malnutrition:
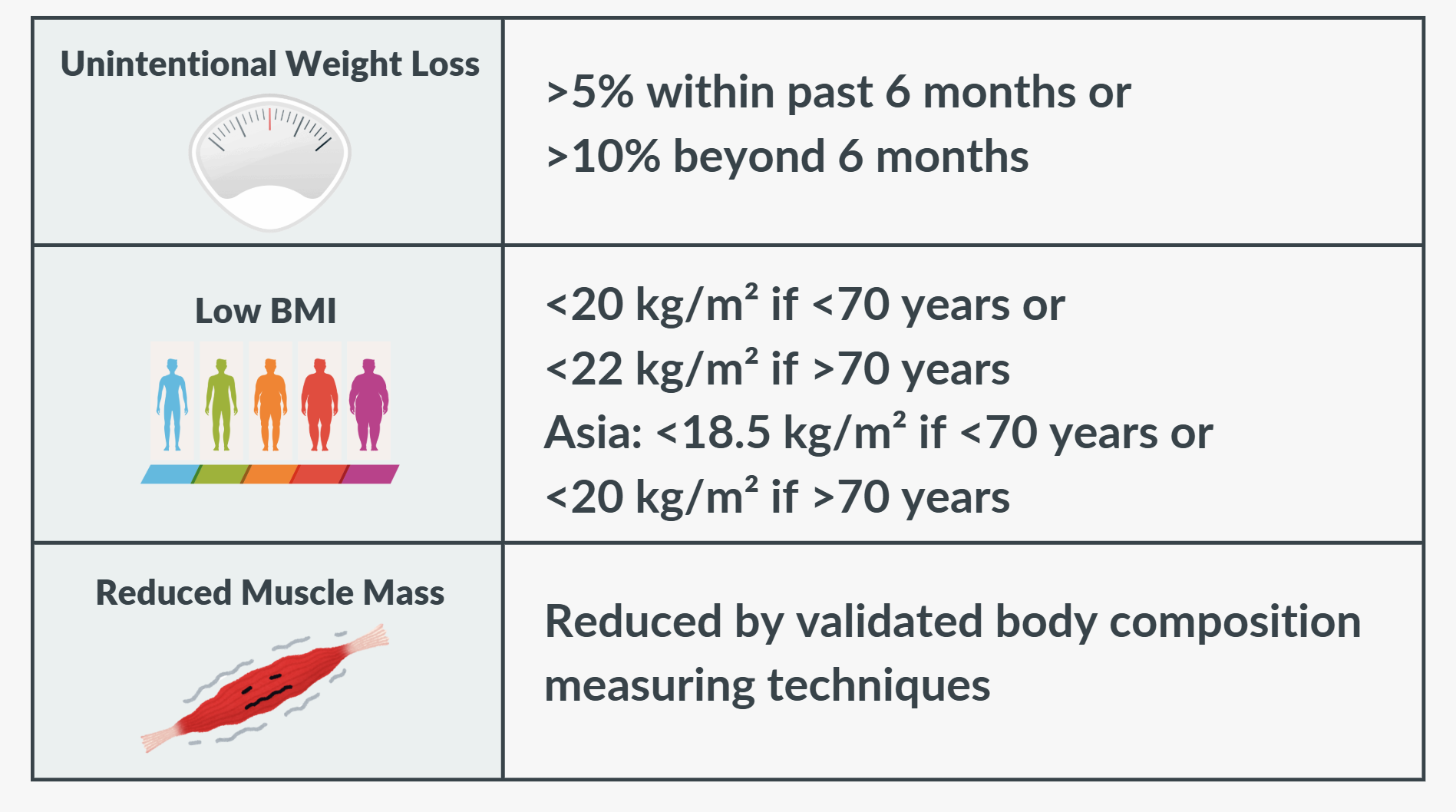 1. Nonvolitional Weight Loss
1. Nonvolitional Weight Loss
Unintentional weight loss is a widely recognized sign of malnutrition. GLIM defines clinically relevant loss as >5% within 6 months or >10% beyond 6 months, considering both acute and chronic changes.
2. Low Body Mass Index (BMI)
A low BMI remains a global marker of malnutrition, even in regions where obesity is common. GLIM recommends cutoffs of <20 kg/m² (<70 years) and <22 kg/m² (>70 years), while for Asian populations, <18.5 kg/m² (<70 years) and <20 kg/m² (>70 years) are advised. However, BMI should be interpreted carefully in individuals with fluid overload or high adiposity, as these may obscure true nutritional status.
3. Low Muscle Mass
The skeletal muscles are the largest organ system in the body and play a vital role in protein metabolism, physical performance, and daily living activities. Adequate energy and protein intake are essential to maintain muscle health — and when these are insufficient, muscle loss becomes one of the most serious consequences of malnutrition.
This loss is often more pronounced in patients with inflammation or severe illness, as muscle catabolism (breakdown) tends to increase during physiological stress.
While the original GLIM consensus did not specify how to define or measure low muscle mass, a GLIM working group later issued practical recommendations to guide implementation in different clinical settings. Because resource availability varies, the choice of method should depend on each institution’s expertise, equipment, and validated cutoffs for the population being assessed.
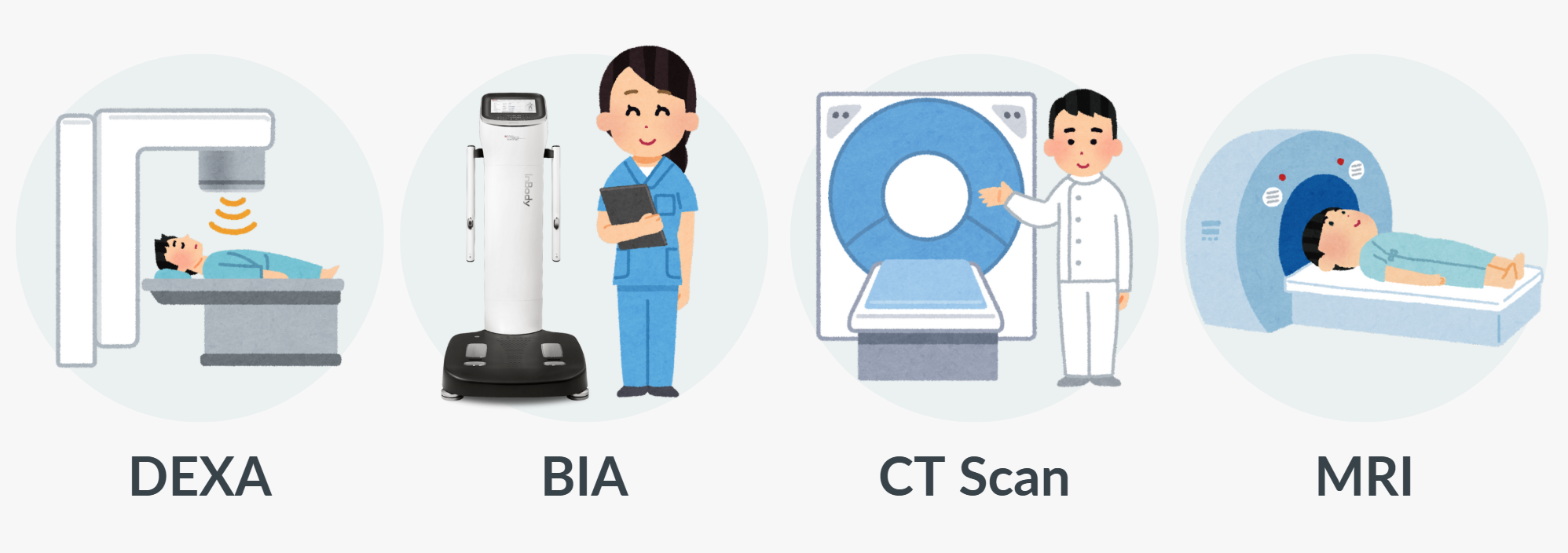
Thus, GLIM recommends several feasible and validated methods, including:
- Dual-energy X-ray absorptiometry (DEXA)
- Bioelectrical impedance analysis (BIA)
- Computed tomography (CT)
- Magnetic Resonance Imaging (MRI)
Source: Cederholm, T., Jensen, G., Correia, M., Gonzalez, M., Fukushima, R., Higashiguchi, T., Baptista, G., Barazzoni, R., Blaauw, R., Coats, A., Crivelli, A., Evans, D., Gramlich, L., Fuchs-Tarlovsky, V., Keller, H., Llido, L., Malone, A., Mogensen, K., Morley, J., . . . Yu, J. (2018). GLIM criteria for the diagnosis of malnutrition – A consensus report from the global clinical nutrition community. Clinical Nutrition, 38(1), 1–9. https://doi.org/10.1016/j.clnu.2018.08.002
Advancing Malnutrition Assessment with InBody Technology
While the GLIM framework defines how malnutrition should be diagnosed, InBody provides the precise tools that translate GLIM’s diagnostic criteria into quantifiable results.
With the advanced InBody S-Series Body Composition Analyzers, including the InBody970S and BWA2.0S, clinicians can objectively evaluate malnutrition risk.
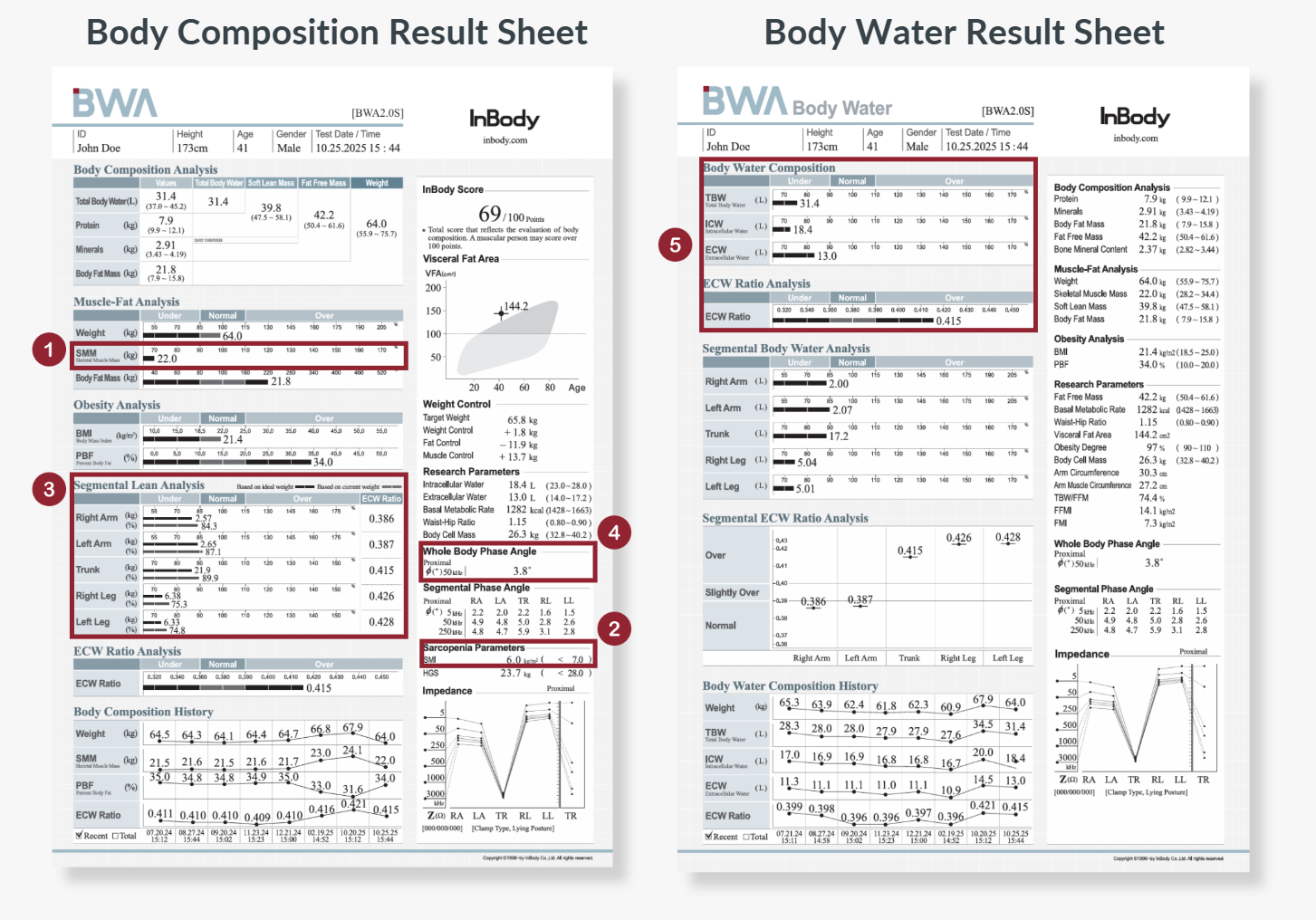 Key InBody Parameters Supporting GLIM Assessment
Key InBody Parameters Supporting GLIM Assessment
- 💪 Skeletal Muscle Mass (SMM)
Represents the total amount of skeletal muscle in the body which is a crucial phenotypic indicator in malnutrition diagnosis. A decline in SMM signals muscle wasting, which may occur due to inadequate nutrition or disease-related catabolism. - 📊 Skeletal Muscle Mass Index (SMI)
Calculated by dividing appendicular lean mass by height squared (kg/m²), SMI provides a standardized measure to assess muscle mass relative to height. Recognized by the Asian Working Group for Sarcopenia (AWGS) as a key diagnostic criterion, SMI plays a crucial role in identifying individuals at risk of sarcopenia and guiding early nutritional and rehabilitative interventions. - 🦵 Segmental Lean Analysis
Provides a visual breakdown of muscle distribution across each limb and the trunk. This helps clinicians identify localized muscle loss or imbalance, offering deeper insight into functional decline and rehabilitation needs. - 🥗 Phase Angle (PhA)
Phase Angle reflects cell membrane integrity and cellular function. A low Phase Angle suggests cell damage, inflammation, or poor nutritional status, and is widely recognized as a predictor of clinical outcomes and recovery potential. - 💦 Body Water Balance (ICW, ECW, ECW Ratio)
InBody measures intracellular and extracellular water directly using multiple low and high frequencies. From this, the ECW Ratio is calculated to assess body water balance. An elevated ECW Ratio may indicate inflammation, edema or severe sarcopenia which are common in conditions like malnutrition, infection, or organ dysfunction.
Conclusion
By integrating the GLIM diagnostic framework with InBody’s precision assessment tools, clinicians can go beyond surface indicators to truly understand each patient’s nutritional status and underlying health.
Because in nutrition care, better assessment leads to better outcomes, and InBody empowers clinicians to make that possible!

Get in touch to bring precision nutrition assessment to your practice!
Learn more about our latest products and how they support precise malnutrition assessment!









