*This webpage content is intended for Healthcare Professionals only, not for general public.
*This webpage content is intended for Healthcare Professionals only, not for general public.
Obesity is no longer viewed as a lifestyle choice, it is now recognized worldwide as a chronic, relapsing disease that demands long-term, evidence-based care.
In recent years, GLP-1 receptor agonists such as semaglutide and tirzepatide have emerged from the diabetes field to transform obesity treatment. These medicines have demonstrated significant efficacy in weight reduction by slowing gastric emptying, blunting hunger signals, and improving insulin sensitivity.
In fact, for many patients, they deliver dramatic weight loss and metabolic improvement, sometimes 15 to 20 percent of body weight in a year. This can be really life-changing for those with obesity and metabolic syndrome.
Yet one question rises beneath the excitement:
What exactly are patients losing — fat, muscle, or water?
The Silent Risk: Muscle Loss During GLP-1 Treatment
For decades, weight loss success has been judged by one number: the reading on the scale. If the number drops, we celebrate. Yet that single metric hides a crucial truth.
Weight loss can come from fat, muscle, or simply water.
This silent risk matters more than ever in the era of GLP-1 medications. These treatments are highly effective at reducing hunger and driving weight loss. However, their appetite-suppressing effect often leads to lower protein intake, which accelerates lean mass loss.
Alarmingly, research shows that up to 40% of total weight lost can come from lean mass when no preventive measures are in place.
And losing muscle is especially harmful because it can:
- Reduce metabolic rate, making it harder to maintain weight loss
- Increase frailty, especially in older adults
- Increase the risk of chronic conditions like diabetes, heart disease, and osteoporosis
From Weight Loss to Body Composition Management
Today, modern obesity management emphasizes:
✅ Reducing fat mass, not just total weight
✅ Preserving lean muscle mass
✅ Enhancing metabolic health and physical function
 This shift from weight-centered to composition-centered care enables clinicians to deliver more personalized, sustainable outcomes — helping patients achieve better health, not just lower numbers.
This shift from weight-centered to composition-centered care enables clinicians to deliver more personalized, sustainable outcomes — helping patients achieve better health, not just lower numbers.
FDA Draft Guidance Highlights Body Composition:
In January 2025, the U.S. FDA recommends incorporating body composition metrics — such as body fat percentage and skeletal muscle mass — alongside traditional measures like total body weight as clinical endpoints.
This policy shift ensures treatment outcomes reflect meaningful physiological changes, not just reductions on the scale.
InBody In Guiding Safe and Effective GLP-1 Weight Loss
Even with highly effective GLP-1 medications, achieving safe and sustainable weight loss requires losing fat while preserving muscle and metabolic health.
So, this is where InBody comes in to make a difference. It provides clinicians with a detailed view of tissue-level changes, helping ensure that weight loss reflects real health improvements, not just numbers on the scale.
Here are the key InBody parameters to follow throughout treatment:
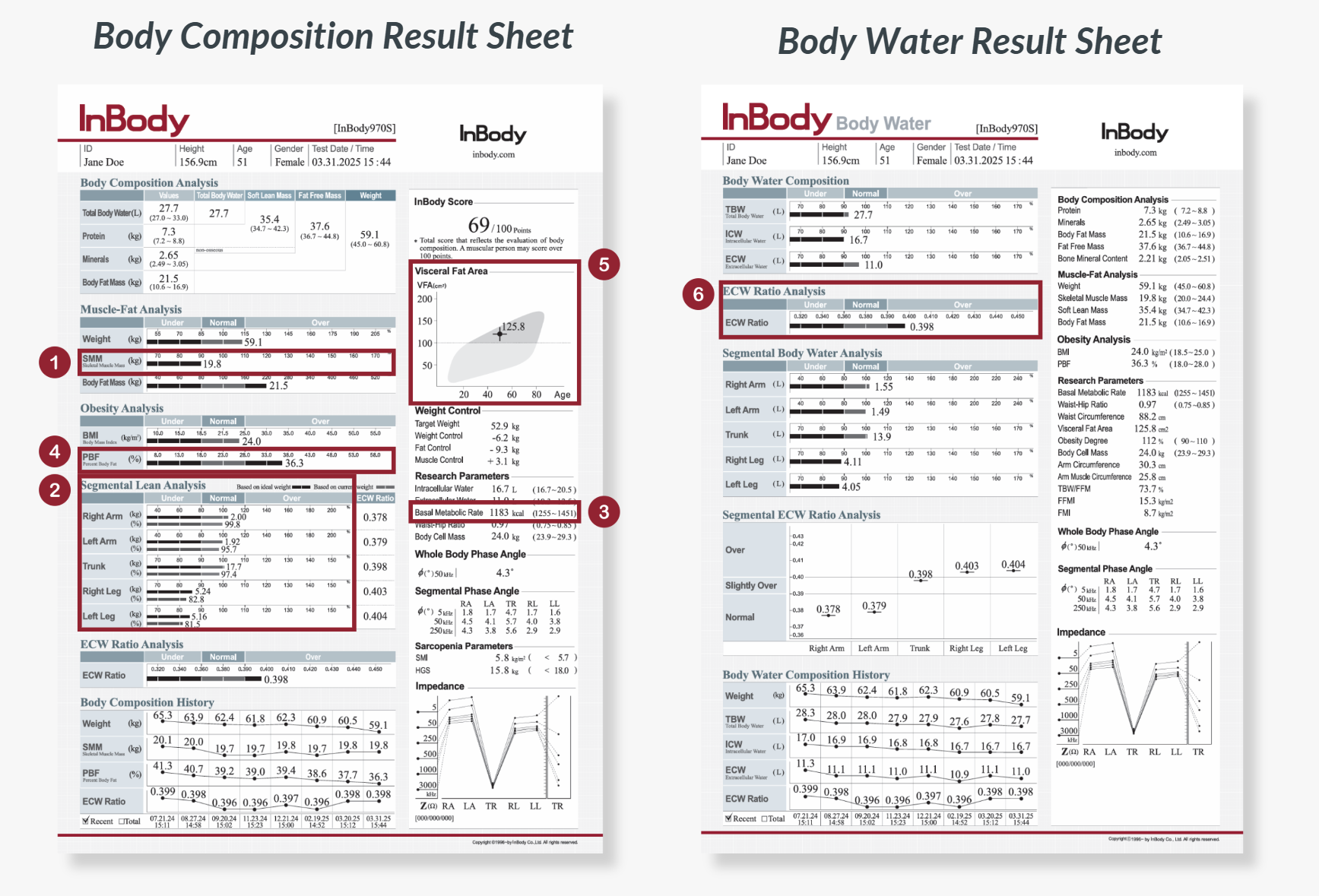
1. Skeletal Muscle Mass (SMM)
Measures total skeletal muscle mass responsible for strength, glucose uptake, and resting energy expenditure. Monitoring SMM ensures weight reduction comes from fat, not the muscle needed to maintain metabolic health and prevent frailty.
2. Segmental Lean Analysis
Shows muscle distribution across each limb and the trunk. It is useful in guiding targeted resistance exercises to preserve muscle where function matters most, especially in older adults vulnerable to sarcopenia.
3. Basal Metabolic Rate (BMR)
Indicates the number of calories needed by the body to sustain basic bodily functions. A declining BMR signals excessive loss of muscle mass, and a higher likelihood of weight regain once medication stops or dosage changes.
4. Percent Body Fat (PBF)
Represents fat relative to total body weight. PBF offers a clearer picture of true obesity improvement, especially when scale weight includes shifts in water.
5. Visceral Fat Area
Measures harmful fat around abdominal organs that drives inflammation, insulin resistance, and cardiovascular disease. GLP-1s specifically target visceral adiposity, making this a crucial marker of treatment success.
6. Extracellular Water (ECW) Ratio
InBody measures intracellular and extracellular water directly using multiple low and high frequencies. From this, the ECW Ratio is calculated to assess body water balance. An elevated ECW Ratio can signal hidden edema that masks true fat-loss progress on the scale, or reflect low-grade inflammation commonly seen in individuals with obesity.
Step by Step: Safe and Sustainable GLP-1 Weight Loss with InBody

Step 1: Baseline Assessment
Before starting treatment, patients undergo a comprehensive InBody Body Composition Analysis to measure skeletal muscle mass, fat mass, body water and other key parameters. This establishes a personalized baseline to track progress over time.
Step 2: GLP‑1 Medication Onboarding
Clinicians prescribe GLP‑1 medications responsibly, starting with low doses and titrating gradually to minimize side effects. Patients receive guidance on protein intake, electrolytes, and hydration, which are critical to preserving muscle while appetite is suppressed.
Step 3: Nutrition and Exercise Interventions
GLP-1 therapy often reduces hunger, which can lead to under-eating, especially protein. Clinicians play a crucial role in supporting patients with structured strategies to preserve muscle and promote healthy weight loss:
- Structured meal planning: A planned approach to nutrition that prioritizes high-quality protein, balanced macronutrients, and appropriate calorie intake to support fat loss while maintaining lean mass
- Resistance training: 2–3 sessions per week targeting major muscle groups
- Low-impact cardio: Walking, cycling, or swimming to support fat loss
This approach focuses on building sustainable habits while ensuring patients maintain muscle mass during treatment.
Step 4: Regular InBody Monitoring
Patients return every 2–4 weeks for follow-up InBody tests to track changes in body composition. This allows clinicians to adjust nutrition, exercise, and medication plans as needed for optimal outcomes.
Conclusion
GLP‑1 therapies are redefining obesity treatment, shifting the focus from weight loss alone to improving body composition, metabolic health, and overall patient outcomes.
With global policies increasingly recognizing body composition as a key endpoint, InBody’s advanced technology provides clinicians and researchers with accurate, repeatable, and actionable insights.
By going beyond the scale, InBody enables a new standard of precision, personalization, and data-driven care in obesity management.
Contact us to discover how InBody can transform your obesity management programs! Watch how InBody drives real results in a clinical weight loss program!